Macular degeneration is a disease that affects the center of the visual field. Central vision is needed for activities like reading, driving, and recognizing people. When looking directly at a person, central vision allows you to be able to see a person’s face and recognize them. In the same way, when watching television, you use your central vision to be able to enjoy the show.
Background
The retina is the light-sensing part of the eye that creates the images you see. The peripheral retina is responsible for motion detection and allowing you to see objects toward the side, such as a person standing at your right or a vehicle approaching at your left. The macula is a small area found in the central retina of the eye. The macula, though very small, plays an important part in vision, because it allows you to see things in fine detail. This sharp vision is sometimes referred to as central vision. Without the macula, tasks like driving, reading and threading a needle would be next to impossible.
What is AMD?
AMD, or Age-Related Macular Degeneration, is usually found in people over 60 years old. Many different factors may contribute to the occurrence of AMD, such as smoking, family history, hypertension, high cholesterol, and a fatty diet, but the primary cause is still not known. Some of the common observations in patients with AMD are the formation of cellular deposits or abnormal blood vessels under the retina.
AMD is described as either wet or dry. The dry form of AMD is most common. This form is milder and develops much more slowly. It occurs when yellow fatty particles known as “drusen” build up underneath the macula. This accumulation of fatty cellular deposits causes damage to some of the macular cells leading to vision loss.
Wet macular degeneration accounts for only about 10 % of AMD cases. While it is more rare, it can cause more serious vision loss and can permanently damage the macula. What happens is that abnormal blood vessels form underneath the retina, where they are not supposed to be present, and cause blood or serous fluid to leak out, resulting in damage to the macula cells and causing vision loss. Wet AMD is usually noticed easily by patients because vision loss occurs rapidly and is more noticeable.
Who is at risk for AMD?
Though the main cause of AMD has not yet been established, research has shown that a number of factors may put people at risk to having this condition. Some of these risk factors are:
- Genetics – Having a family member who has AMD may put you are at a higher risk of acquiring the condition. Studies suggest that having a variant of a certain gene called Complement Factor H (CFH) accounts for 43% of AMD cases.
- Constant exposure to oxidative stress – Every day our body reacts with the free oxygen around us. The end products of these reactions are called free radicals, tiny particles that can react with our cells and tissues and, over time, can cause damage on the cellular level. Exposure to these free radicals is called oxidative stress and is assumed to increase the chance of having macular degeneration.
- Obesity, high cholesterol levels, and high blood pressure – Patients with these conditions have been shown to have higher chances of acquiring AMD. In men, abdominal obesity has been observed to be a risk factor.
- Fatty diets – High amounts of saturated fat in the diet contribute to the development of AMD.
- Smoking – Cigarette smoking raises the risk of having AMD about three times.
Various studies confirm the link between cigarette smoking and AMD, suggesting that smoking has harmful effects on the retina.
What are the signs/symptoms of AMD?
Patients with dry AMD usually do not recognize the condition until an eye examination is done or until vision loss is more noticeable. Patients who have AMD may have the following signs or symptoms:
- Blurring, haziness, shadows or holes in the vision, especially at the center of vision
- Straight lines appearing wavy
- Trouble seeing details both up close and at a distance
- Difficulty telling colors apart, especially those close in hue
- Trouble recognizing people’s faces
- Slower than usual vision recovery after exposure to bright lights


How is it diagnosed?
The key to treating AMD is having your ophthalmologist diagnose the condition as early as possible. There are different ways of diagnosing AMD depending on how serious the presenting symptoms are.
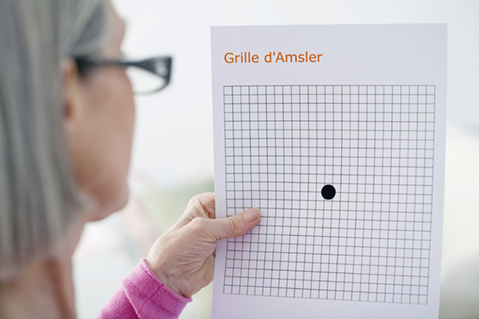
For dry macular degeneration, an examination with an ophthalmoscope is done. Regular and thorough examination of the retina is important once you have a diagnosis of dry macular degeneration. Your ophthalmologist will first administer eye drops to cause your pupils to widen. This is for easy visualization of the inner structures of the eye with the ophthalmoscope. If your doctor sees any abnormalities in the macula, you will be asked to monitor your vision using a chart called an Amsler Grid. An Amsler Grid allows you to easily observe any changes in your vision. Using the Amsler grid every day will help you monitor if there are any changes in your vision, especially because dry macular degeneration can progress into the more severe wet form. Any changes in vision, such as lines becoming distorted, or parts of the grid becoming dark or hazy, should be immediately reported to your ophthalmologist.
If your ophthalmologist thinks that you may have wet macular degeneration, he or she may perform tests such as fluorescein angiography (FA) and optical coherence tomography (OCT). Fluorescein angiography involves the injection of a dye into your veins, which combines with the blood and flows into blood vessels including those found in the retina. As the dye passes through blood vessels in the eye, it can be photographed with a special camera and can demonstrate abnormalities in the retinal circulation or tissue structure of the retina. This information will then be used to determine where the abnormal blood vessels are and how they can be treated. Optical coherence tomography (OCT) scanning uses infrared laser light to scan the retina. OCT is able to detect small amounts of fluid or swelling in the retina as well as checking for any irregularities in the tissue layers of the macula.
How is it treated?
Sadly, there are no available treatments yet for dry macular degeneration. If you are a patient having one or more risk factors for AMD, a checkup with your ophthalmologist is advised every one to two years. Early detection of dry AMD can help you and your doctor come up with ways by which you can slow down and prevent its progression. First, cutting back on fat intake and avoiding habits that put you at risk can help slow down AMD. Moreover, certain patients can benefit from eye vitamins, also called AREDS vitamins, which can help prevent the transformation from dry AMD to wet AMD.
The use of these AREDS vitamins comes from large, National Institutes of Health sponsored studies, entitled “Age-Related Eye Disease Study (AREDS).” The most recent of these studies shows that people at high risk of developing wet macular degeneration can substantially lower their risk of progression by at least 25%. These supplements did not appear to benefit those without the more advanced form of dry AMD with high-risk features. Please note that these vitamins do not cure macular degeneration; nor can they replace any vision that was previously lost. Rather, the goal of the supplements is to prevent the transformation of the dry into the wet kind of AMD which usually results in more serious and rapid vision loss.
The most recent formulation of these supplements per the AREDS2 study should include:
- Vitamin C (500 mg)
- Vitamin E (400 International Units, IU)
- Lutein (10 mg)
- Zeaxanthin (2 mg)
- Zinc Oxide (80 mg)
- Copper / Cupric oxide (2 mg)
Other studies have shown that eating dark, leafy greens, as well as brightly colored vegetables (e.g. red, orange) which are rich in zeaxanthin and lutein, may also decrease the risk of development of macular degeneration. Finally another large study in women showed that folic acid and Vitamin B6 / B12 may benefit your ocular health.
For wet macular degeneration, there is still no total cure, but several treatments are currently available to combat the disease and prevent it from causing severe and total vision loss. Some treatments are:
Laser photocoagulation – This treatment uses a thermal laser to seal abnormal blood vessels and prevent them from leaking any further. The downside to this treatment is that the laser may leave a scar and cause a permanent blind spot. This is the reason why this procedure is rarely performed and is only used in patients who are willing to lose a part of their visual area to save remaining vision.
Photodynamic therapy – A light-activated drug is injected into the vein and a “cold laser” is used to activate the drug in the affected area. Upon activation, the drug acts to block the leaking blood vessels. Unlike the first option, this treatment does not leave a scar and may be performed as many times as necessary.
Anti-angiogenesis drugs – These drugs are categorized as “anti-vascular endothelial growth factor” drugs or anti-VEGF. They act to block proteins from playing a role in the growth of abnormal blood vessels.
Your ophthalmologist will discuss the best diagnostic and treatment options with you depending on your problem and will work with you to prevent further progression of the disease. Schedule an appointment with your ophthalmologist today!
