Glaucoma
Glaucoma is a characteristic pattern of optic neuropathy and in most cases, has no symptoms until late in the course of the disease. Risk factors for glaucoma include family history of glaucoma, history of ocular trauma, age over 60 years old, chronic steroid use in any form including eyedrops, creams, and pills, and African/Hispanic ancestry. The mainstay of treatment in glaucoma is to lower the intraocular pressure to a level at which further damage to the optic nerve does not occur. This “target” pressure can vary depending on the person and the status of the optic nerve.
Open Angle Glaucoma
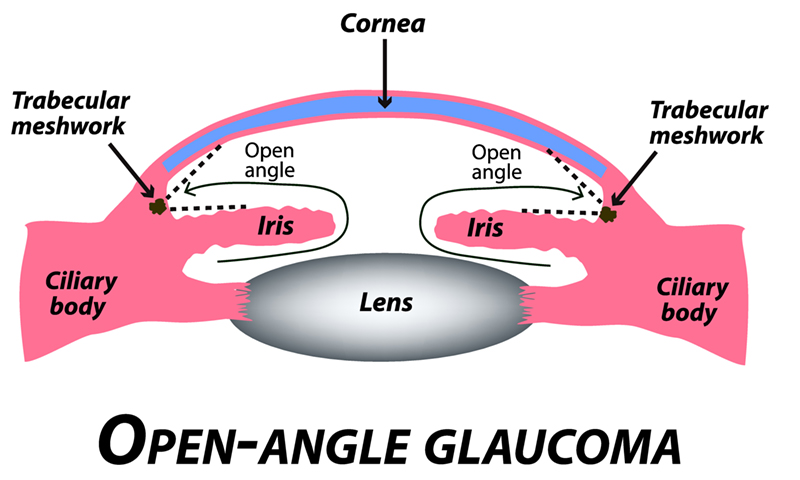
In open angle glaucoma, treatment options include trabeculoplasty (also termed ALT, SLT), topical or oral medications (generics include timolol, brimonidine, dorzolamide, latanoprost, acetazolamide), or outpatient surgery (Minimally Invasive Glaucoma (MIGS) procedures, trabeculectomy with or without mitomycin C, glaucoma shunt surgery, cyclophotocoagulation).
Narrow Angle Glaucoma
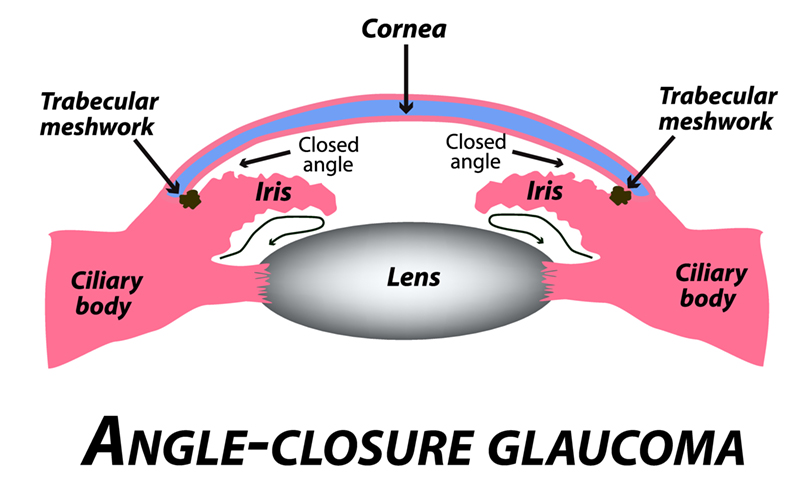
In narrow angle glaucoma, the iris is physically too close to the drainage structures and thereby obstructs aqueous leaving the eye. As a result, the intraocular pressure is elevated. Generally, an office-based laser peripheral iridotomy is recommended at this point. It is important to realize that even after an iridotomy is done and the angle is more “open”, the angle can narrow again in the future. Cataract surgery or iridoplasty can be done if this situation arises.

